Many business leaders believe Good Samaritan laws provide a blanket of legal protection just for having an AED on-site. However, that protection is almost always conditional. To be shielded from liability, your organization must prove it has followed every rule in your state’s statute, from regular inspections to proper team training. One missed check or an expired battery could put your legal immunity at risk. A well-managed program is your best defense, and it all starts with a clear understanding of the AED requirements for businesses. Let’s break down what you need to do to ensure your program is truly compliant.
Key Takeaways
- Treat Your AED as a Program, Not Just a Product: An AED’s effectiveness depends on a complete readiness system. This includes strategic placement for quick access, consistent maintenance checks, and ensuring it’s prepared to function correctly in an emergency.
- Compliance Is Your Best Defense Against Liability: State laws offer legal protection, but it’s conditional. Following all rules for maintenance, training, and documentation is essential to shield your organization from negligence claims and fines.
- Document Everything to Prove Readiness: Meticulous records of inspections, supply expiration dates, and team training are non-negotiable. This documentation is your proof of due diligence during an audit or in the event of an incident.
Why Does Your Business Need an AED?
When you think about workplace safety, fire extinguishers and first-aid kits probably come to mind. But what about the single most effective tool for responding to a sudden cardiac arrest (SCA)? An Automated External Defibrillator (AED) isn’t just a piece of medical equipment; it’s a lifeline that can mean the difference between life and death for an employee, a customer, or a visitor. Having an AED on-site is one of the most impactful decisions you can make for the well-being of everyone in your facility.
Beyond the profound moral responsibility to protect your people, a well-managed AED program is a cornerstone of modern corporate safety and risk management. It demonstrates a clear commitment to preparedness and can significantly reduce legal and financial liability. The reality is that sudden cardiac arrest can happen to anyone, at any time, regardless of age or health status. When it does, the clock starts ticking immediately. Having an AED accessible and ready to use empowers your team to act decisively in those critical first few minutes before emergency medical services (EMS) can arrive. Let’s break down exactly why this device is so essential.
How AEDs Save Lives During Cardiac Arrest
Sudden cardiac arrest occurs when the heart’s electrical system malfunctions, causing it to stop beating effectively. An AED is designed to fix this specific problem. The device analyzes the heart’s rhythm and, if it detects a life-threatening arrhythmia, delivers a controlled electrical shock to restore a normal heartbeat. It’s the only definitive treatment for SCA. The impact is staggering: a Johns Hopkins study found that when a victim receives AED treatment before EMS arrives, their chance of survival can increase from a national average of about 8% to 38 percent. Modern AEDs are incredibly user-friendly, providing clear voice and visual prompts to guide anyone through the process, making it possible for any bystander to save a life.
Why Every Second Counts
During a cardiac arrest, time is the most critical factor. For every minute that passes without a defibrillating shock, a person’s chance of survival drops by 7-10%. While calling 911 is the first step, the average response time for paramedics can often exceed the narrow window for a successful outcome. An on-site AED bridges that crucial gap. Having a device immediately available allows your team to intervene while help is on the way, dramatically improving the odds. Simply put, placing an AED in your facility gives a person experiencing SCA the best possible chance at survival by putting life-saving technology in the hands of those closest to the emergency.
Protecting Your People and Your Business
Implementing an AED program is a powerful way to show your employees and customers that you prioritize their safety. It fosters a culture of care and preparedness that resonates with everyone who enters your building. From a business perspective, it’s also a critical component of risk management. While many organizations install AEDs voluntarily, some states and industries have specific laws requiring them. Properly maintaining your AED and adhering to local regulations is key to insulating your business from potential liability. A comprehensive AED program management plan ensures your device is always ready, your team is prepared, and your organization is protected.
Is an AED Legally Required for Your Business?
The short answer is: it depends. While you won’t find a sweeping federal law that requires every business to have an automated external defibrillator (AED), the legal landscape is a patchwork of state and local regulations. For many organizations, the question isn’t just about a legal mandate but about liability, safety, and doing the right thing for your employees and customers.
Understanding your specific obligations is the first step. Federal bodies like the Occupational Safety and Health Administration (OSHA) provide guidance, but the real requirements are often found in your state’s laws. These rules can be surprisingly detailed, covering everything from where an AED must be placed to how often it needs to be inspected. On top of that, certain industries face stricter requirements than others. Navigating these rules is key to not only ensuring safety but also protecting your organization from potential negligence claims. The good news is that Good Samaritan laws offer a layer of legal protection, but that protection often hinges on having a well-managed and compliant AED program.
Understanding Federal and OSHA Guidance
Let’s start at the top. Currently, there is no federal law that requires all businesses to have an AED on-site. OSHA encourages workplaces to include AEDs as part of their first-aid and emergency response programs, but it stops short of a mandate for most industries. Instead, federal guidance focuses on ensuring a safe workplace, which can be interpreted to include readiness for cardiac emergencies, especially in high-risk environments.
Because there isn’t a single federal rule, the responsibility falls on individual states to set their own standards. This is why you can’t assume you’re in the clear just because OSHA doesn’t have a specific AED requirement for your industry. The most important regulations you’ll need to follow will almost always be at the state or even local level.
A Look at State-Specific AED Laws
This is where compliance gets complicated. Nearly every state has laws related to AEDs, but they vary dramatically. Some states only require them in specific locations, while others have broader legislation. These laws often come with a detailed list of requirements for any business that chooses to implement an AED program. This can include registering your device with local emergency services, performing regular maintenance checks, and ensuring proper signage.
Many of these state laws offer legal immunity to businesses, but this protection is usually conditional. To be protected from a lawsuit, you often have to prove you followed every single rule in the statute. Missing an inspection or failing to replace expired pads could put your organization’s immunity at risk. You can find a helpful overview of AED requirements by state to see what your local obligations are.
Rules for Industries like Gyms, Schools, and Public Venues
While not all businesses are required to have an AED, some industries are held to a higher standard due to the nature of their activities or the number of people they serve. State laws frequently single out specific types of facilities and mandate that they have AEDs readily available. These often include:
- Schools and universities
- Gyms, fitness centers, and health clubs
- Dental offices and other healthcare facilities
- Large public venues like stadiums and concert halls
- Government buildings and airports
If your business falls into one of these categories, it’s critical to research your state’s specific laws. The requirements are often non-negotiable and may dictate the number of devices needed, staff training protocols, and placement for optimal accessibility.
How Good Samaritan Laws Offer Protection
All 50 states have Good Samaritan laws designed to protect bystanders who step in to help during a medical emergency. These laws were created to encourage people to act without fear of being sued if their efforts are unsuccessful. In most cases, this protection extends to the use of an AED.
For a business, these laws can also provide a shield from liability, but it’s not automatic. This legal protection is often tied directly to the management of your AED program. If your device was not properly maintained, its batteries were dead, or your staff wasn’t trained, that immunity could disappear. A compliant, well-documented AED program management system is your best defense, ensuring your organization is protected when you provide a life-saving device.
What Happens if You Don’t Comply with AED Laws?
Placing an AED in your facility is a critical first step, but the responsibility doesn’t end there. State and federal laws include specific rules for maintenance, training, and documentation. Falling short on these requirements can create serious problems for your organization, turning a life-saving device into a significant liability. Ignoring these rules not only puts lives at risk but also exposes your business to legal and financial consequences that are entirely avoidable. Let’s walk through what can happen when an AED program isn’t managed correctly.
The Risk of Liability and Negligence Claims
One of the biggest risks of non-compliance is being exposed to a negligence lawsuit. If someone suffers a cardiac arrest at your facility and the AED fails to work because of a dead battery, expired pads, or improper maintenance, your organization could be held responsible. Many business owners believe that simply having an AED protects them, but the opposite can be true if the device isn’t ready for use. Courts have shown that providing a faulty AED can be considered worse than providing none at all. To protect your organization, you must demonstrate that you’ve followed all maintenance and readiness protocols outlined in your state’s laws.
Facing Fines and Regulatory Penalties
Beyond civil lawsuits, failing to comply with AED regulations can lead to direct fines and penalties from state or local authorities. While federal OSHA guidance is less specific, many states have strict laws that mandate AEDs in certain types of businesses, such as gyms, schools, and large public venues. For example, states like California and Illinois require health clubs to have AEDs because of the higher risk of sudden cardiac arrest during exercise. If your business falls into one of these categories and you fail an inspection or don’t meet the requirements, you could face costly citations. These penalties are designed to enforce compliance and ensure public safety, making them a serious financial concern for any business owner.
Losing Your Legal Immunity
Most states have Good Samaritan laws that offer legal protection to organizations that provide and use AEDs in good faith. However, this immunity is almost always conditional. To be protected, you must follow every requirement in your state’s AED statute, which can include device registration, routine inspections, and staff training. According to legal experts, failing to comply with even a single rule could cause you to forfeit your immunity from negligence claims. This means one missed inspection or one expired set of pads could be all it takes to expose your organization to a devastating lawsuit. Maintaining meticulous records and a consistent maintenance schedule is your best defense.
Failing Audits and Creating More Work
A poorly managed AED program creates ongoing administrative headaches. Whether it’s an internal safety audit or an official inspection, your program’s records will be scrutinized. If you can’t produce documentation proving your AEDs are properly maintained, registered, and inspected, you will fail the audit. This outcome does more than just look bad on paper; it triggers a cascade of extra work. You’ll likely be required to create a corrective action plan, undergo follow-up inspections, and dedicate significant time and resources to fixing the gaps in your program. This diverts focus from your core business operations and adds unnecessary stress for your entire team.
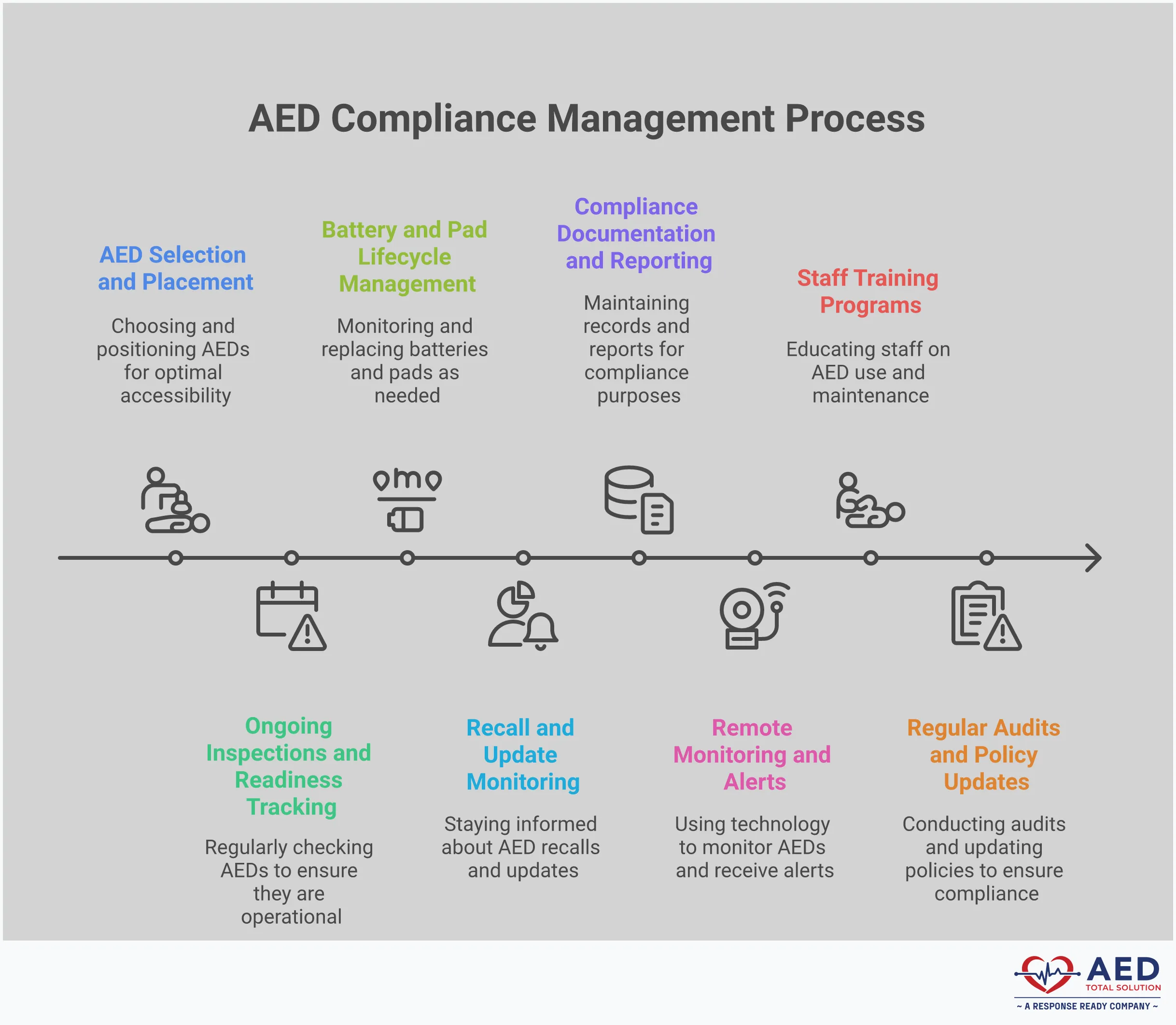
How to Build a Compliant Workplace AED Program
Putting a compliant AED program in place is more than just buying a device and mounting it on the wall. It’s about creating a complete system that ensures your AED is always ready and your team is prepared to act. A strong program protects your employees, reduces liability, and gives everyone peace of mind. Building one from the ground up involves a few key steps, from strategic placement and team training to diligent maintenance and record-keeping.
Think of it as a readiness plan. Each component works together to close compliance gaps and make sure your investment in safety truly pays off when it matters most. By following a structured approach, you can create a program that is not only compliant with regulations but also genuinely effective in an emergency. Let’s walk through the essential steps to get your program up and running.
Place Your AEDs for Quick Access
Where you put your AED is just as important as having one. During a cardiac arrest, every second is critical, so the device needs to be easy to find and grab. Place your AEDs in central, high-traffic locations like lobbies, break rooms, or near elevators. The goal is for someone to be able to retrieve the AED and return to the victim within three minutes.
Make sure the AED is clearly visible and not hidden in a closet or an unmarked cabinet. Use standardized signage to point the way from multiple directions. This ensures that even visitors or new employees can locate it quickly in a high-stress situation. A well-placed AED is the first step toward a successful response.
Train Your Team to Respond Confidently
An AED is designed to be used by almost anyone, with clear voice prompts guiding the user. However, panic can be a major obstacle in an emergency. Providing your team with formal training in CPR and AED use builds the confidence they need to step in and act decisively. This training helps them understand the “why” behind each step and prepares them to respond effectively.
Regular refresher courses keep these life-saving skills sharp. When employees feel prepared, they are far more likely to use the AED correctly, manage the scene, and provide critical care until professional help arrives. A well-trained team transforms a piece of equipment into a true life-saving program.
Create a Maintenance and Inspection Schedule
An AED is a medical device that requires regular attention to stay ready for use. You can’t just set it and forget it. A consistent maintenance schedule is essential for compliance and readiness. This involves routinely checking that the indicator light is green, confirming that electrode pads and batteries have not expired, and ensuring supplies are fully stocked.
Most AEDs perform daily self-tests, but monthly visual inspections are a best practice. It’s also important to stay on top of manufacturer notices or recalls. A comprehensive AED program management service can automate these checks, tracking expiration dates and inspection logs to ensure your device is always prepared for an emergency.
Establish Medical Oversight and Management
Most state laws require an AED program to be managed under the guidance of a physician. This is known as medical oversight. A medical director provides a prescription for the device, reviews protocols, and helps ensure your program follows established best practices. They can also review event data after the AED is used to provide feedback and ensure quality control.
This oversight is a critical piece of a compliant and medically sound program. It connects your workplace response efforts to the broader emergency medical system, ensuring your team is providing care that aligns with professional standards. It’s a layer of assurance that protects both the victim and your organization.
Master Your Documentation and Record-Keeping
If it isn’t written down, it didn’t happen. Meticulous documentation is your proof of compliance and a key part of limiting liability. You should keep detailed records of everything related to your AED program, including monthly inspection logs, battery and pad expiration dates, training certificates for your volunteer responders, and any maintenance performed.
These records are essential for passing audits and demonstrating due diligence. In the event of an incident, having a complete and organized file shows that you have responsibly managed your program. Centralized, audit-ready reporting simplifies this process, giving you a clear view of your program’s status at all times.
Plan Your Budget for Long-Term Readiness
The initial purchase of an AED is just one part of the overall investment. To maintain a state of readiness, you need to budget for ongoing costs. These include replacing electrode pads and batteries every two to five years, running regular training sessions for your team, and covering the cost of program administration and medical oversight.
Factoring these recurring expenses into your budget from the start ensures your program remains effective and compliant for the long haul. For predictable costs, some organizations choose an AED rental or a full-service management plan that bundles equipment, maintenance, and support into one consistent fee.
Related Articles
- AED Laws & Requirements Across State — AED Total Solution
- Mastering Life-Saving Devices: Why AEDs Are Crucial — AED Total Solution
- Florida AED Statutes & Regulations — AED Total Solution
- Texas AED Statutes & Regulations — AED Total Solution
- Pennsylvania AED Statutes & Regulations — AED Total Solution
Frequently Asked Questions
If my state doesn’t legally require an AED for my business, why should I still get one? While your state may not mandate an AED, the decision to have one is about more than just checking a legal box. It’s a fundamental part of workplace safety and risk management. Sudden cardiac arrest can happen to anyone, and having an AED on-site dramatically increases a person’s chance of survival. It shows your employees and customers that you are prepared to protect them, which builds a strong culture of care. From a business standpoint, it also reduces your liability by demonstrating a commitment to safety.
What’s the difference between just buying an AED and having a full AED program? Buying the device is only the first step. A full AED program is the complete system that ensures the device is ready to use at a moment’s notice. This includes everything from strategic placement and staff training to regular maintenance checks, supply replacement tracking, and medical oversight. A comprehensive program addresses all the legal and readiness requirements, making sure your AED is an asset that protects people, not a liability collecting dust on a wall.
Can any employee use an AED, or is special training required? Modern AEDs are designed to be incredibly simple, with clear voice prompts that guide a user through every step. In an emergency, anyone can and should use one. However, providing formal CPR and AED training is a crucial part of a compliant program. Training gives your team the confidence to act quickly and correctly under pressure, helping them overcome the hesitation that can cost precious seconds. It prepares them to manage the scene effectively until paramedics arrive.
Are Good Samaritan laws enough to protect my business from a lawsuit? Good Samaritan laws offer important legal protections, but they aren’t a blank check. This immunity is almost always tied to you properly managing your AED program according to your state’s specific rules. If an AED fails because of a dead battery or expired pads, that legal protection could be voided. The best way to ensure you are protected is to maintain meticulous records of your inspections, maintenance, and training.
What is the most common reason an AED fails during an emergency? The most frequent and preventable cause of AED failure is a lack of maintenance. This usually comes down to two simple things: an expired battery or expired electrode pads. AEDs perform regular self-checks, but if no one is physically inspecting the device and tracking these expiration dates, it can easily become unusable without anyone realizing it. A consistent inspection schedule is the only way to guarantee your AED is ready when you need it most.
Disclaimer for information purposes only:
The information provided on this website is intended for general educational and informational purposes only. It is not medical advice and should not be used as a substitute for professional diagnosis, treatment, or care. Always consult a qualified healthcare or medical professional regarding any health-related questions or concerns.
While we strive to ensure the information shared is accurate and up to date, no guarantees are made regarding completeness, accuracy, or applicability to any individual situation. Use of this content is at the reader’s sole discretion and risk.
This website is part of the Response Ready family of emergency preparedness and training resources, including CPR & first aid training and compliance services, AED sales and program support, AED program management software, and medical oversight solutions provided through our affiliated platforms:
• CPR1.com
• AEDLeader.com
• ResponseReady.com
• MDSIMedical.com
By accessing or using this website, you agree to release, indemnify, and hold harmless the website owners, authors, contributors, and affiliated entities from any claims, losses, damages, or liabilities arising from the use or reliance on the information presented.