In a sudden cardiac arrest, the clock is your biggest enemy. A person’s chance of survival drops dramatically with every minute that passes. The goal is to get an AED to their side and deliver a shock within three to five minutes. This critical window should be the driving force behind your entire placement strategy. While the AED location requirements OSHA suggests are flexible, the science of survival is not. Placing your AEDs strategically is less about checking a compliance box and more about engineering a rapid response. We’ll show you how to map your facility to meet this timeline and ensure your program is built for speed.
Key Takeaways
- Make Your AED Reachable in Under 3 Minutes: Place devices in visible, unlocked, and high-traffic areas to ensure a rescuer can retrieve and apply the AED within the critical survival window.
- An AED is Only Ready if You Maintain It: Go beyond placement by creating a consistent schedule for physical inspections, tracking battery and pad expiration dates, and keeping detailed compliance records.
- Formalize Your Program to Eliminate Guesswork: A written emergency response plan and an audit-ready documentation system are non-negotiable for ensuring compliance and reducing liability.
What Does OSHA Say About AED Placement?
When you’re setting up an AED program, one of the first questions that comes to mind is, “What are the rules?” Many people look to the Occupational Safety and Health Administration (OSHA) for clear-cut answers, but the guidance can feel a bit gray. While OSHA doesn’t have a specific standard that requires every single employer to have an AED, its regulations point toward the need for one in many workplaces.
The core of OSHA’s stance is rooted in ensuring a safe work environment. This includes having a plan for medical emergencies, especially for sudden cardiac arrest. OSHA’s guidelines are designed to be flexible, but they consistently emphasize that emergency equipment must be accessible and ready for immediate use. The agency strongly encourages the installation of AEDs in workplaces as a critical part of a first-aid program. Think of it less as a strict mandate and more as a powerful recommendation that aligns with best practices for employee safety and risk management. A well-placed AED isn’t just about checking a compliance box; it’s about creating a response-ready culture that can save a life when seconds count.
What is OSHA’s Role in AED Placement?
OSHA’s primary role is to ensure employers provide a safe workplace. While there isn’t a one-size-fits-all rule for AEDs, OSHA does require that medical services and first aid are “readily available” for employees, particularly when there isn’t a hospital or clinic in close proximity. This is where AEDs become essential. For many businesses, an on-site AED is the most effective way to meet this requirement for cardiac emergencies. The term “readily available” implies that life-saving equipment can be reached and used within minutes, which is critical for surviving a sudden cardiac arrest.
Key OSHA Guidelines for AEDs
The most important OSHA guideline for AEDs is simple: they must be accessible. If you choose to have an AED program, the device can’t be locked away in an office or stored in a hard-to-reach closet. OSHA emphasizes that AEDs should be placed in locations that are visible and available to everyone during all working hours. This means choosing central, high-traffic spots like lobbies, break rooms, or main hallways. The goal is to minimize the time it takes for someone to retrieve the device and bring it to the person in need, making a swift response possible.
Common Myths About OSHA’s AED Rules
A common myth is that you only need an AED if OSHA explicitly mandates it for your industry. In reality, many organizations implement AED programs because it’s a responsible safety measure that protects their team and reduces liability, regardless of a specific rule. Another dangerous misconception is that any placement is good enough. Sticking an AED in a manager’s office that gets locked after 5 p.m. renders it useless for employees working later shifts. An AED must be accessible to all, all the time. Proper program management ensures these critical details are never overlooked.
What’s the Ideal AED Response Time?
When someone experiences sudden cardiac arrest (SCA), the clock starts ticking immediately. Having an AED in your building is the first step, but its effectiveness hinges on how quickly your team can get it to the person in need. This isn’t just about having the right equipment; it’s about having a response plan built for speed. The time it takes to recognize the emergency, retrieve the AED, and deliver a shock is the single most important factor in determining the outcome.
So, what’s the magic number? While every situation is different, safety experts and regulatory bodies have established clear benchmarks for an effective AED response. Understanding this timeline helps you move from simply owning an AED to creating a truly life-saving program. Below, we’ll break down the critical time window for AED use, explore how response time directly impacts survival rates, and give you practical steps for mapping out your AED locations to ensure your device is always within reach when seconds matter most.
The Critical 3-5 Minute Window
The widely accepted standard for an effective AED response is three to five minutes. This isn’t just a suggestion; it’s a critical benchmark for survival. According to OSHA guidance, your AEDs should be placed so that a trained responder can retrieve the device and apply it to a victim within this short window. Think of it as your “drop-to-shock” time. From the moment a person collapses, your goal is to have a defibrillator at their side and ready to use in under five minutes. This timeline accounts for everything—recognizing the emergency, calling for help, grabbing the AED, and applying the pads.
How Response Time Impacts Survival
Why is the 3-5 minute window so important? The data is sobering. For every minute that passes without CPR or a shock from an AED, a person’s chance of surviving sudden cardiac arrest drops by 7% to 10%. After just five minutes, survival rates can decrease by as much as 50%. By the 10-minute mark, the chances of survival are tragically low. This statistic highlights the urgency of a rapid response. An AED stored in a locked office or a distant corner of your facility might as well not be there at all. A fast response is the key to giving someone the best possible chance.
How to Map Out Your AED Coverage
To meet the 3-5 minute goal, you need to be strategic about where you place your AEDs. Start by walking through your facility and identifying high-risk and high-traffic areas. Think about places where people gather, like lobbies, cafeterias, and conference rooms, as well as areas with strenuous activity, such as fitness centers or manufacturing floors. Your workplace AED program should ensure a device is always accessible. A good rule of thumb is the “90-second rule”: a person should be able to walk to an AED from anywhere in your building in 90 seconds or less. This leaves enough time to return to the victim and apply the device within the critical window. And remember, never place an AED in a locked room or office—it must be accessible to everyone during all hours of operation.
Key Factors for Smart AED Placement
Once you understand the importance of response time, the next step is strategic placement. It’s about more than just mounting a box on a wall; it’s about creating a network of accessible, life-saving devices. A well-placed AED can be the difference between a close call and a tragedy. While OSHA provides a framework, smart placement considers the unique layout and risks of your specific environment. Let’s walk through the key factors that ensure your AEDs are not just present, but perfectly positioned for an emergency.
Make it Visible and Easy to Access
An AED that can’t be found is an AED that can’t be used. Visibility is your first priority. Place your devices in prominent, central locations where people naturally gather or pass by, like reception areas, break rooms, or main hallways. Use clear, universally recognized signage to point the way from multiple directions. The path to the AED should be completely unobstructed—no boxes, furniture, or equipment in the way. It’s also critical to ensure the AED is never behind a locked door. When an emergency happens, no one should have to waste precious seconds searching for a key or a manager. Our AED program management services can help you map out these key locations for maximum visibility and access.
Identify High-Risk and High-Traffic Zones
Where is a sudden cardiac arrest most likely to happen in your facility? Start by identifying high-traffic zones where a large number of people congregate, such as cafeterias, auditoriums, or busy production floors. Next, consider high-risk areas where individuals might experience physical stress. This could be a company gym, a manufacturing line, or any space where strenuous activity occurs. Placing AEDs closer to these locations shortens the distance a rescuer needs to travel, helping you meet that critical three-to-five-minute response window. A thorough site assessment is the best way to pinpoint these crucial spots and ensure your AED coverage is truly effective, leaving no gaps in your emergency response plan.
Meet ADA Height and Accessibility Standards
Accessibility means accessible for everyone. When installing your AED cabinet, it’s essential to follow the Americans with Disabilities Act (ADA) guidelines to ensure anyone, including individuals in wheelchairs, can reach the device. The rule of thumb is to mount the cabinet so that the highest operable part (like the handle) is no more than 48 inches from the floor. This simple step ensures that a potential rescuer isn’t stopped by a physical barrier. Make sure the area in front of the cabinet is kept clear, allowing for easy approach and access. You can find a variety of compliant AED cabinets and accessories that meet these standards while keeping your device secure.
Protect Your AED from the Elements and Theft
Your AED is a sensitive piece of medical equipment that needs protection to function correctly. A durable cabinet is non-negotiable for shielding the device from dust, moisture, and accidental damage. If you’re placing an AED outdoors, near a pool, or in an industrial setting, you’ll need a specialized cabinet designed to withstand extreme temperatures and weather conditions. To prevent tampering or theft, consider using an alarmed cabinet. The alarm sounds when the door is opened, which not only deters misuse but also helps alert others nearby that an emergency is in progress. Regular inspections and maintenance are crucial to confirm that both the AED and its protective housing are in perfect working order.
How to Keep Your AEDs Ready for Action
Placing an AED in a visible, accessible spot is a great first step, but the work doesn’t stop there. An AED is only effective if it’s ready to work at a moment’s notice. This means regular maintenance, diligent record-keeping, and a clear system for ensuring every device is functional and compliant. Without a solid readiness plan, even the best-placed AED can fail when it’s needed most, creating significant liability for your organization.
Think of it like a fire extinguisher—you trust it’s ready, but that trust is built on a system of regular checks and maintenance. Your AED program requires the same level of attention. From tracking expiration dates on pads and batteries to performing routine inspections and documenting every action, keeping your devices ready is an ongoing commitment. Let’s walk through the essential steps to ensure your AEDs are always prepared for an emergency, giving you and your team true peace of mind.
Keep Clear Compliance Records
Managing an AED program involves more than just mounting a device on the wall. To stay compliant and prepared, you need to maintain clear, organized records for every AED you own. This documentation is your proof that you are responsibly managing your life-saving equipment. Your records should include inspection logs, maintenance reports, battery and pad replacement dates, and staff training certifications. These documents are essential for internal audits and can be critical in demonstrating due diligence. A well-documented program shows you’re proactive about safety, which helps reduce organizational liability and ensures you meet state and local requirements.
Track Battery and Pad Expiration Dates
An AED’s battery and electrode pads have finite shelf lives, and using expired components can cause the device to fail during a rescue. According to OSHA guidance, employers must maintain AEDs according to the manufacturer’s specifications, which always includes monitoring expiration dates. Make it a priority to create a system for tracking these dates for every device in your inventory. Set calendar reminders or use a spreadsheet, but be aware that manual tracking can become difficult to manage, especially with multiple AEDs. Having a reliable system ensures you can order and install replacement batteries and pads before they expire, keeping your devices in a constant state of readiness.
Create a Regular Inspection Schedule
Consistent, routine inspections are the backbone of a reliable AED program. Don’t just wait for an alert or an upcoming expiration date. Establish a regular schedule—typically monthly—to physically check each AED. During an inspection, you should confirm the status indicator light is green, check that supplies like pads and razors are present and intact, and ensure the device hasn’t been tampered with or damaged. Each inspection should be logged in your compliance records. This simple, repeatable process helps you catch potential issues early and reinforces that your AEDs are always ready for action.
Consider Remote Monitoring for Peace of Mind
While manual inspections are essential, they only provide a snapshot in time. What happens between those checks? Remote monitoring technology can fill that gap by automatically checking the AED’s status every single day. These systems send real-time alerts if the device’s status changes, a battery is running low, or the cabinet is opened. This gives you immediate insight into the health of your entire AED fleet without requiring daily physical checks. For organizations with multiple locations, this technology is a game-changer, providing centralized oversight and ensuring every device is ready. It’s a key part of a comprehensive program management strategy that adds a powerful layer of security and confidence.
How to Overcome Common AED Program Challenges
Even with the best intentions, managing an AED program can present a few common hurdles. From devices hidden in locked offices to inconsistent training, these issues can undermine your entire emergency preparedness plan. The good news is that these challenges are entirely solvable with a bit of planning and the right strategy. Let’s walk through how to tackle the most frequent obstacles to ensure your program is effective, compliant, and always ready to help save a life.
Solve Common Placement and Access Issues
One of the biggest mistakes organizations make is poor AED placement. An AED tucked away in a manager’s locked office or a remote supply closet is useless during an emergency. The goal is to make the device easy to find and grab within seconds. Think about central, high-traffic areas like lobbies, break rooms, or near elevators. The key is accessibility for everyone, at all times. As OSHA guidance suggests, AEDs should be placed in locations that are readily available in case of an emergency, not just during standard business hours. A simple walkthrough of your facility can help you spot and fix these critical access issues.
Train Your Team and Raise Awareness
Having an AED is only half the battle; your team needs the confidence to act. An effective program includes regular training on both CPR and AED use. A one-time session isn’t enough—skills get rusty, and people forget what to do under pressure. Building a culture of preparedness means making training an ongoing priority. You can host drills, share informational posters, and ensure everyone knows where the AEDs are located. When people feel prepared, they are far more likely to step in and help, turning a moment of panic into a coordinated and effective response.
Simplify Compliance for Multiple Locations
Managing one AED has its challenges, but overseeing devices across multiple buildings or cities adds layers of complexity. Tracking different state regulations, inspection schedules, and supply expiration dates for each location can quickly become overwhelming. This is where a centralized system becomes essential. Managing an AED program is much more than just buying a device and mounting it on a wall. A comprehensive approach ensures every device in your portfolio is compliant and ready. Using an AED program management service can streamline everything, giving you a single source of truth for your entire program and peace of mind that nothing is falling through the cracks.
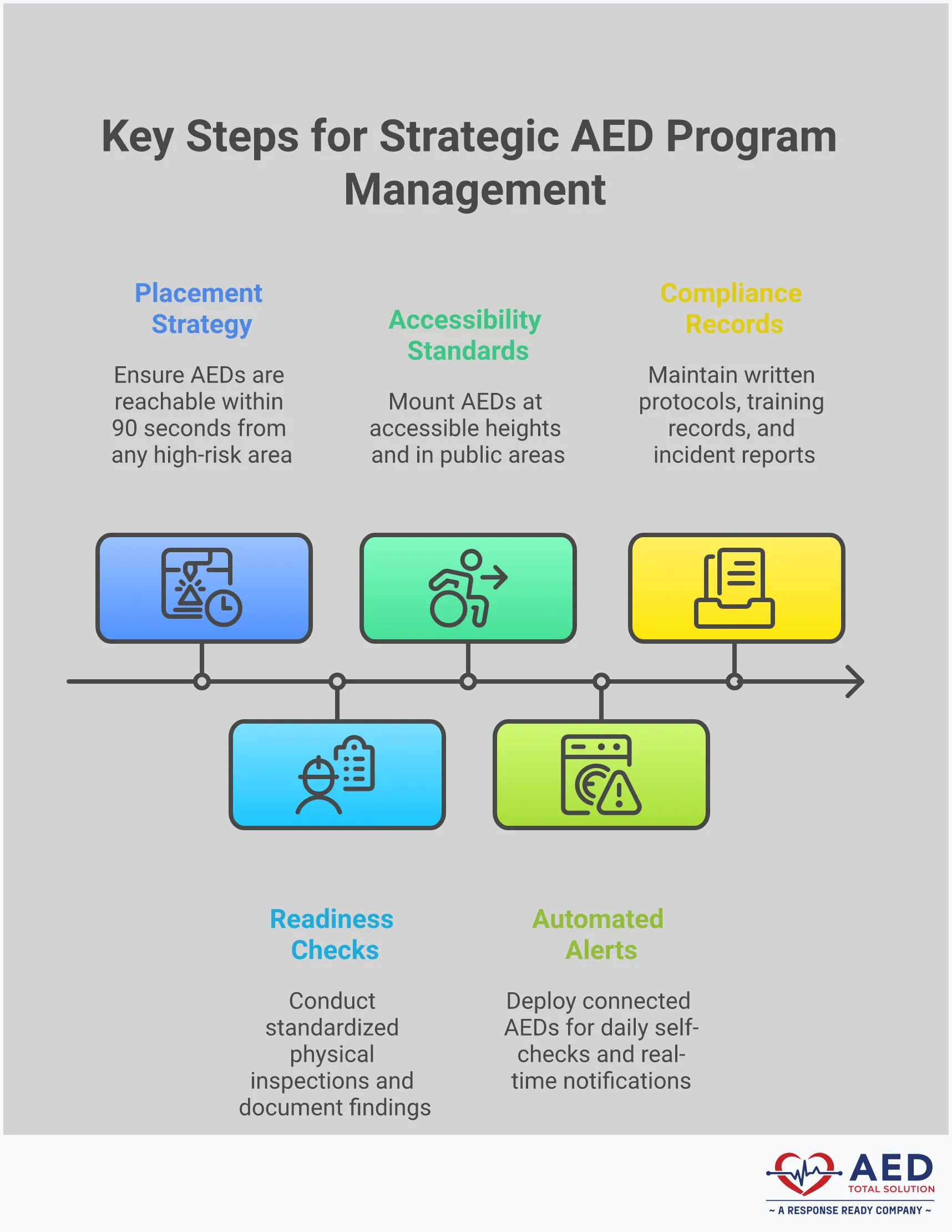
How to Build a Strong AED Program Strategy
A truly effective AED program goes beyond just placing devices on walls. It’s built on a clear strategy that covers everything from initial assessment to ongoing maintenance and team readiness. A well-defined plan not only ensures your AEDs are ready when needed but also protects your organization from compliance gaps and liability risks. It turns your AEDs from simple equipment into a reliable, life-saving system.
Creating this strategy involves three key steps: understanding your unique risks, defining your response plan, and maintaining meticulous records. By thinking through each of these areas, you can build a program that is both compliant and genuinely prepared to handle a sudden cardiac arrest emergency.
Start with a Workplace Risk Assessment
Before you decide where to place an AED, you need to understand your environment’s specific needs. A workplace risk assessment helps you identify potential hazards and high-risk areas. Start by reviewing your organization’s OSHA incident reports to see where accidents have occurred in the past. Think about your workforce demographics, the physical layout of your facility, and the nature of the work being done.
You can also get valuable advice from local emergency services or healthcare professionals who can offer an expert perspective on your site. The goal is to create a clear picture of where a cardiac emergency is most likely to happen, ensuring your AEDs are placed for maximum impact. This foundational step informs every other part of your program.
Define Your Emergency Response Plan
Once you know your risks, you can create a written emergency response plan. Think of this as your playbook for a sudden cardiac arrest event. This plan should be a formal document that details every aspect of your AED program. According to OSHA guidelines, this plan should outline where your AEDs are located, who is responsible for maintaining them, and who is trained to use them.
Your plan should also include protocols for what happens when an AED is used, such as calling 911, starting CPR, and retrieving the device. It’s crucial to assign clear roles and responsibilities so everyone knows what to do in a high-stress situation. A comprehensive plan ensures your team can act quickly and confidently, turning a chaotic moment into a coordinated response.
Set Up an Audit-Ready Documentation System
Managing an AED program is an ongoing responsibility, not a one-time task. To stay compliant and ensure readiness, you need a reliable system for tracking everything. This means keeping detailed records of routine inspections, battery and pad expiration dates, and any maintenance performed, all in line with the manufacturer’s instructions.
This documentation is your proof of compliance and is essential for any audit. An organized system helps you stay ahead of maintenance schedules and demonstrates that you are actively managing your program. Whether you use a digital platform or a detailed logbook, having an audit-ready documentation system is a non-negotiable part of responsible AED program management. It provides peace of mind that your devices are always ready and your organization is protected.
When to Partner with an AED Program Manager
Keeping up with AED placement, maintenance, and documentation can feel like a full-time job, especially when you’re juggling other safety and compliance responsibilities. If your program is growing, spread across multiple locations, or you simply want confidence that every detail is covered, it might be time to work with an AED program manager. This partnership isn’t just about offloading tasks; it’s about implementing a professional system to protect your people and your organization.
An expert partner can help you move from simply having AEDs to managing a truly response-ready program. They handle the complex details of compliance and readiness, giving you the freedom to focus on your core responsibilities while knowing your emergency plan is solid.
The Benefits of Full Program Oversight
Managing an AED program involves much more than just buying a device and mounting it on a wall. It requires ongoing maintenance, regular staff training, and compliance with a web of local and state regulations. Without dedicated oversight, it’s easy for critical tasks to slip through the cracks, like replacing expired electrode pads or updating your registration after moving a device.
Full program oversight means having an expert dedicated to every aspect of your AED program’s lifecycle. A program manager tracks maintenance schedules, monitors device status, and ensures every unit is compliant and ready for use. This white-glove approach to AED program management removes the administrative burden from your team and significantly reduces your organization’s liability risk. You gain peace of mind knowing that a professional is making sure your program is always prepared for an emergency.
How Integrated Systems Simplify Management
For many organizations, AEDs are tracked using spreadsheets or calendar reminders, which are prone to human error and quickly become unmanageable as a program grows. An integrated AED management system can streamline the process of tracking device locations, maintenance schedules, and training records, ensuring that your program remains compliant and effective. These systems provide a single source of truth for every device you own.
Instead of manually checking on each AED, you can use a central dashboard to see the status of your entire fleet at a glance. Automated alerts will notify you of upcoming battery expirations or missed inspections, while audit-ready reports can be generated with a few clicks. This combination of smart software and expert support makes it simple to answer common questions about your program’s health and prove compliance whenever needed.
Get Expert Support for All Your Locations
The complexity of an AED program multiplies with each new location. Ensuring compliance and readiness across different buildings, cities, or even states introduces logistical hurdles and requires knowledge of varied local regulations. A decentralized approach often leads to inconsistent maintenance, incomplete documentation, and gaps in compliance from one site to the next.
If you need support with setup, maintenance, or training, partnering with an AED program manager can provide the expertise necessary to ensure compliance across multiple locations. They can standardize your emergency response plan, manage device inspections remotely, and coordinate service for every site. Whether you need to purchase new devices or arrange an AED rental for a temporary facility, an expert partner provides a scalable solution that grows with you, ensuring every location is equally prepared.
Related Articles
- AED Program Management | Compliance and Maintenance
- AED Laws & Requirements Across State — AED Total Solution
- AED Laws & Requirements Across State — Florida AED Statutes & Regulations
- AED Signage Requirements and Laws to Ensure Legal Compliance
Frequently Asked Questions
Is my business legally required to have an AED? While OSHA doesn’t have a blanket rule that forces every business to own an AED, its requirement for “readily available” first aid often makes having one a practical necessity. Some states and local governments do have specific laws for certain industries, like gyms or schools. The most important thing to remember is that having an AED program is a best practice for protecting your team and reducing liability, regardless of whether a specific rule applies to you.
How many AEDs do I actually need for my building? There isn’t a magic number, as the answer depends entirely on your facility’s layout. The goal is to get the AED to a person within three to five minutes. A good way to plan is to use the “90-second walk” rule: can someone get from any point in your building to an AED in 90 seconds or less? This gives them enough time to return to the person in need. You should consider factors like multiple floors, secured areas, and sprawling wings to ensure you have adequate coverage.
My AED’s status light is green. Is that enough to know it’s ready? A green light is a great start, but it doesn’t tell the whole story. The AED’s self-test confirms the battery has a charge and the internal circuits are working, but it can’t tell you if the electrode pads are expired or if the rescue kit is missing supplies. That’s why regular, hands-on inspections are so important. You need to physically check that the pads and batteries are within their use-by dates and that the device is clean and accessible.
We have AEDs at several locations. What’s the biggest mistake to avoid? The most common pitfall for multi-location organizations is inconsistent management. It’s easy for one site to have a perfectly maintained program while another location completely neglects its device, leaving it with expired pads or a dead battery. This creates a huge gap in safety and a major liability. The key is to have a single, centralized system for tracking inspections, supplies, and compliance for every single device, ensuring a consistent standard of readiness everywhere.
What’s the difference between just tracking my AEDs and having a managed program? Tracking is a passive task, like noting expiration dates on a spreadsheet and hoping someone remembers to act on them. A managed program is an active, comprehensive system. It means having an expert who ensures inspections are completed on time, follows up on device alerts, manages all documentation, and confirms that every AED is not just monitored, but truly ready to be used in an emergency. It shifts the responsibility from a line item on a checklist to a fully supported, life-saving system.
Disclaimer for information purposes only:
The information provided on this website is intended for general educational and informational purposes only. It is not medical advice and should not be used as a substitute for professional diagnosis, treatment, or care. Always consult a qualified healthcare or medical professional regarding any health-related questions or concerns.
While we strive to ensure the information shared is accurate and up to date, no guarantees are made regarding completeness, accuracy, or applicability to any individual situation. Use of this content is at the reader’s sole discretion and risk.
This website is part of the Response Ready family of emergency preparedness and training resources, including CPR & first aid training and compliance services, AED sales and program support, AED program management software, and medical oversight solutions provided through our affiliated platforms:
• CPR1.com
• AEDLeader.com
• ResponseReady.com
• MDSIMedical.com
By accessing or using this website, you agree to release, indemnify, and hold harmless the website owners, authors, contributors, and affiliated entities from any claims, losses, damages, or liabilities arising from the use or reliance on the information presented.