A well-intentioned AED program can fail for a few simple, avoidable reasons. A device hidden in a locked office, a battery that died months ago, or a team that hesitates in a crisis can render your investment useless. These common mistakes create a false sense of security and can have devastating consequences. The key to avoiding them is understanding that a successful program is about more than just hardware; it’s about creating a complete system of readiness. This guide highlights the most frequent pitfalls and shows you how to avoid them by properly addressing all aed installation requirements, from visible placement and team training to consistent maintenance checks and documentation.
Key Takeaways
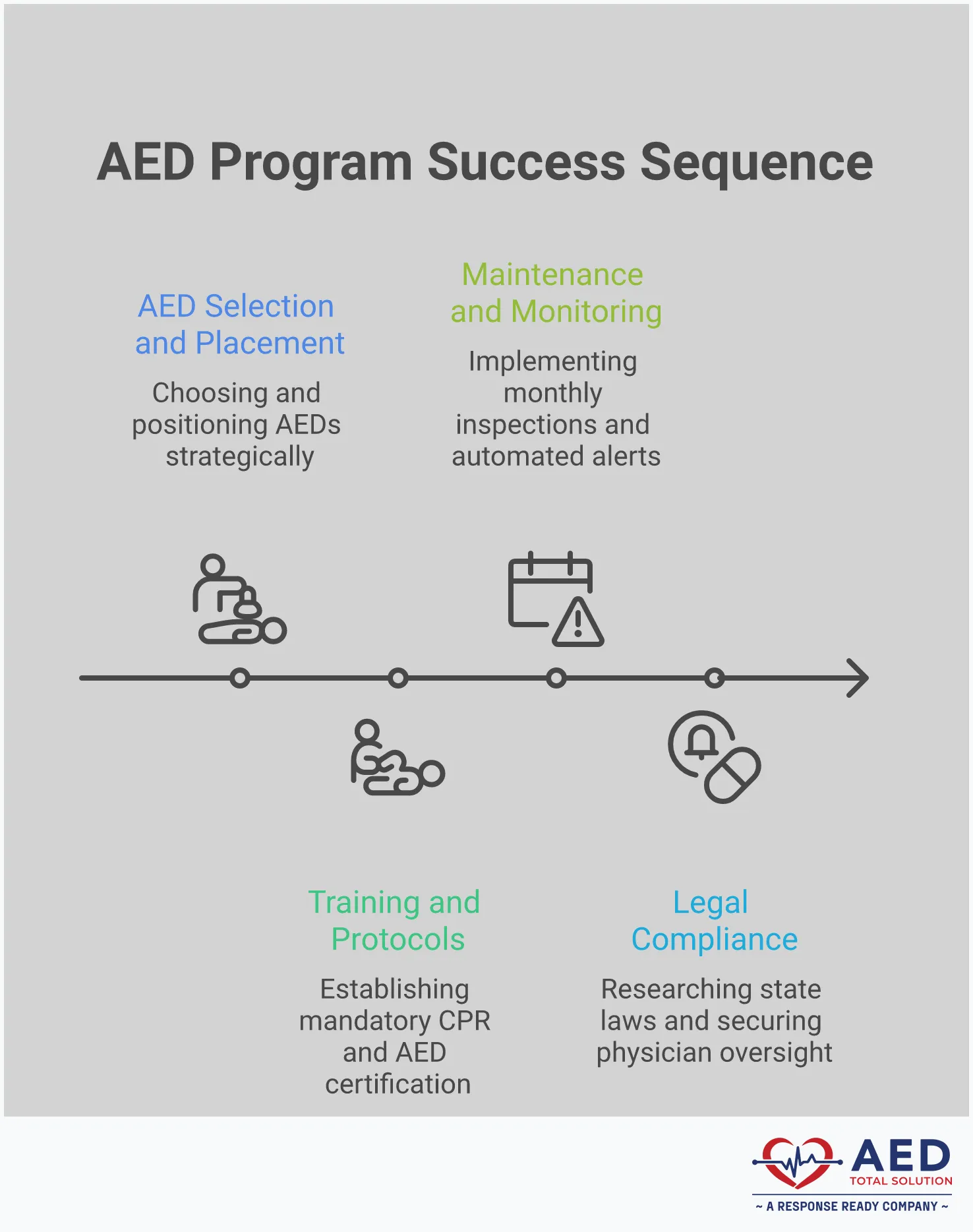
- Build your program on a solid foundation: A successful AED program starts with understanding your specific legal requirements, using the three-minute response rule to determine the right number of devices, and placing them in visible, accessible, and central locations.
- Empower your team to act with confidence: A device is only as good as the people prepared to use it. Ensure your program includes certified CPR and AED training, hands-on practice drills, and a clear emergency response plan that outlines everyone’s role during a crisis.
- Commit to ongoing management for guaranteed readiness: Avoid the common mistake of “set it and forget it.” A reliable program requires consistent monthly inspections, diligent tracking of battery and pad expiration dates, and audit-ready documentation to ensure your AED is always functional.
What Are the Legal Requirements for AEDs?
Figuring out the legal side of AED ownership can feel like untangling a knot. There isn’t one single law that covers every business in every state. Instead, compliance is a mix of federal recommendations, specific state laws, and rules for certain industries. Getting a handle on these requirements is the first step to building an AED program that not only saves lives but also protects your organization from liability.
Think of it in three layers: federal guidance sets the stage, state laws provide the specific rules for your location, and industry standards add another level of requirements you might need to follow. While it sounds complicated, breaking it down makes it much more manageable. Understanding these legal pieces ensures your program is built on a solid foundation, giving you confidence that your devices are ready and your organization is protected. Let’s walk through each layer so you know exactly what applies to you.
Federal Guidelines and OSHA Recommendations
While there’s no federal law that forces every business to have an AED, the Occupational Safety and Health Administration (OSHA) strongly encourages them as a critical part of workplace safety. OSHA views having an AED program as a best practice, especially for businesses where the risk of sudden cardiac arrest is higher or where emergency medical services might take longer to arrive.
The agency emphasizes that acting quickly with CPR and an AED is the key to survival. Because of this, OSHA recommends that employers install these devices and, just as importantly, provide proper training for employees on how to use them. Following these guidelines helps create a safer environment for everyone and shows a commitment to employee well-being.
State-Specific Laws and Registration
This is where AED compliance gets more specific. The rules for AEDs can vary significantly from state to state. Some states mandate AEDs in certain types of facilities, like gyms, schools, or large public venues. Others have broader requirements or simply encourage their placement.
A key part of many state laws is AED registration. You may be required to register your device with your local emergency medical services (EMS) agency. This allows 911 dispatchers to direct a bystander to your AED in an emergency. Additionally, most states have Good Samaritan laws that offer liability protection to organizations and individuals who use an AED in good faith to help someone. It’s essential to research your state’s specific requirements to ensure you’re fully compliant.
Industry-Specific Requirements
On top of federal and state rules, your specific industry might have its own requirements for AEDs. For example, many states have passed laws requiring AEDs in all schools and at school-sponsored athletic events. Healthcare facilities, dental offices, and fitness centers often face specific mandates regarding the placement and maintenance of AEDs.
These industry-specific regulations are designed to protect the public in environments where the risk of cardiac arrest may be higher or where large groups of people gather. As you develop your AED program, be sure to check for any rules that apply directly to your field. Staying informed about these standards is crucial for maintaining compliance and ensuring you’re meeting the expected standard of care for your industry.
How Many AEDs Does Your Facility Need?
Deciding on the right number of AEDs for your organization isn’t about meeting a simple quota; it’s about creating a life-saving system that works in the real world. When a sudden cardiac arrest occurs, every second is critical. The number of devices you need is directly tied to how quickly a rescuer can get one to the person in need. A single, poorly placed AED in a large building might as well not be there at all.
The goal is to ensure that anyone, anywhere in your facility, can retrieve an AED and return to the victim within three minutes. This principle, known as the three-minute response rule, should be the foundation of your placement strategy. To figure out your magic number, you’ll need to consider your facility’s unique layout, size, and potential barriers. A thoughtful site assessment is a key part of any effective AED program management plan and ensures your devices are positioned for the fastest possible response.
The Three-Minute Response Rule
The three-minute response rule is the industry standard for a reason. For every minute that passes without defibrillation, a person’s chance of survival drops by about 10%. The American Heart Association recommends delivering a shock within three to five minutes of collapse for the best outcome. This window includes everything from someone recognizing the emergency to retrieving the AED, applying the pads, and delivering the shock.
To meet this guideline, a rescuer should be able to get to the AED and back to the victim in under three minutes. This is often called the “drop-to-shock” time. Basing your AED count on this simple but powerful rule ensures your program is built for speed and effectiveness when it matters most.
Facility Size and Occupancy
The physical size of your building is the first factor to consider. While a common guideline is to have at least one AED per floor in a multi-story building, this isn’t a one-size-fits-all solution. The real test is the three-minute walk. Time yourself walking from the furthest point of an area to the proposed AED location and back again at a brisk pace. If the roundtrip takes longer than three minutes, you need another AED to cover that zone.
Also, think about where people gather. High-occupancy areas like cafeterias, auditoriums, fitness centers, or busy lobbies are high-risk zones. These locations should have their own dedicated AED, even if another device is technically within a three-minute walk, to avoid delays caused by crowds.
Planning for Multiple Floors and Buildings
A straight line on a floor plan doesn’t reflect a real-world emergency response. When you perform your three-minute walk-through, be sure to account for any physical barriers that could slow a rescuer down. This includes stairs, elevators (which may not be usable during an emergency), locked doors, security checkpoints, or even cluttered hallways. Each of these obstacles adds precious seconds to your response time.
If you manage a campus with multiple buildings, treat each one as its own facility requiring a separate assessment. An AED in the main office does little good for someone in a warehouse across the parking lot. For organizations needing to cover several locations, exploring an AED rental program can be a flexible way to scale your device count without a large upfront investment.
Where Should You Place Your AEDs?
Deciding where to install your AEDs is one of the most critical parts of setting up your program. An AED that’s locked away or hidden in a closet won’t do anyone any good. The goal is to place your devices in locations that are visible, accessible, and central to where people spend their time. When sudden cardiac arrest strikes, every second counts, and a well-placed AED can dramatically shorten the time to the first shock. Strategic placement ensures that a rescuer can grab the device and return to the patient’s side within that crucial three-minute window.
Place AEDs in High-Traffic and Central Locations
Think about the natural pathways and gathering spots in your building. Lobbies, cafeterias, main corridors, and employee break rooms are all excellent candidates for AED placement. You want the device to be in a location that people pass by every day, making it familiar and easy to find in an emergency. Certain areas also carry a higher risk for cardiac events, such as fitness centers or large assembly halls. Prioritizing these high-risk locations ensures that help is closest where it’s most likely to be needed. The key is to position your AEDs for the shortest possible retrieval time from any point in your facility.
Follow ADA Accessibility Guidelines
Your AED must be accessible to everyone, including individuals with disabilities. Following the Americans with Disabilities Act (ADA) guidelines is not just a matter of compliance—it’s about ensuring anyone can be a rescuer. The ADA has specific rules for wall-mounted objects like AED cabinets. To maintain a clear path, the cabinet cannot stick out more than four inches from the wall. For height, the handle of the AED should be no more than 48 inches from the floor for a forward approach. This ensures that a person in a wheelchair can safely reach and retrieve the device without assistance.
Ensure AEDs Are Visible with Clear Signage
An AED is useless if no one knows it’s there. Visibility is everything. Your AED should be housed in a clearly marked, unobstructed cabinet. Don’t hide it behind a plant or around a blind corner. Use universally recognized AED signage to draw attention to its location. Installing a 3D sign that projects from the wall above the cabinet helps people spot it from a distance or down a long hallway. The goal is to make your AED so easy to find that even a first-time visitor could locate it in a panic. Clear and consistent signage is a simple step that saves precious time.
What Training Does Your Team Need?
Placing an AED on the wall is a great first step, but your work isn’t finished. For your program to be effective, your team needs to feel confident and ready to act during an emergency. Sudden cardiac arrest is chaotic and stressful, and hesitation can cost precious seconds. Proper training turns bystanders into capable responders, ensuring the device is used quickly and correctly.
A well-rounded training program goes beyond just knowing which button to press. It builds a culture of safety and preparedness, empowering your staff to handle a crisis. This involves three key components: getting certified in CPR and AED use, practicing with hands-on drills, and establishing a clear emergency response plan that everyone understands. By investing in your team’s skills, you ensure your AED is more than just a piece of equipment—it’s a lifeline ready to be used.
CPR and AED Staff Certification
Effective AED use starts with foundational knowledge. That’s why comprehensive training should always cover both how to operate an AED and how to perform cardiopulmonary resuscitation (CPR). During a certification course, your team will learn how to assess an emergency, identify the signs of sudden cardiac arrest, and operate the device safely and effectively.
While modern AEDs provide clear voice prompts, formal training removes the guesswork and builds the confidence needed to act decisively under pressure. A certified responder knows not to wait. They understand the importance of chest compressions and how the AED works with their efforts to restore a normal heart rhythm. Reputable organizations like the American Heart Association offer courses that prepare your team for a real-world emergency.
Schedule Hands-On AED Practice
Watching a video or reading a manual isn’t enough to prepare someone for a cardiac emergency. Hands-on practice is essential for building muscle memory so your team can take immediate action without freezing. An onsite training session allows employees to get comfortable with the specific AED model in your facility, from opening the case to applying the electrode pads.
This practical experience is invaluable. It gives your designated responders a chance to run through emergency scenarios and practice the proper techniques for adults, children, and infants. Regular drills help keep these skills sharp and ensure your emergency response team works together seamlessly. When everyone knows their role, your program becomes far more effective.
Develop an Emergency Response Plan
A formal emergency response plan is the backbone of your entire AED program. This document outlines exactly what to do when someone suffers a sudden cardiac arrest in your facility. It should detail a clear sequence of events: who calls 911, who retrieves the AED, who begins CPR, and who directs emergency services when they arrive. This protocol is a critical component of your program’s medical oversight.
Your plan should be written, accessible, and reviewed regularly with your team. It should also integrate with your facility’s other safety procedures, such as your bloodborne pathogens exposure control plan. A well-documented plan not only prepares your team but also demonstrates that you have a compliant, well-managed program in place.
How to Manage Registration and Documentation
After your AED is installed, the work isn’t over. Proper registration and documentation are what make your AED program legally sound and effective. Think of it as the essential administrative backbone that supports your life-saving hardware. This paperwork protects your organization from liability and gives your team the confidence that every protocol has been followed. It’s your official record proving that you are responsibly managing your device and are prepared for an emergency. This isn’t just about checking boxes; it’s about creating a system of accountability that ensures your AED is ready to perform when seconds matter most.
From registering the device with local authorities to tracking every maintenance check, these steps create a clear, traceable history of your AED’s readiness. A well-documented program shows you’re proactive about safety and compliance, which is critical in the event of an audit or after an incident. While managing these details can feel like a lot, especially for organizations with multiple locations, it’s a non-negotiable part of ownership. This is why many businesses partner with an AED program management service to ensure every detail is handled correctly and nothing falls through the cracks, giving you peace of mind that your program is always protected and audit-ready.
Fulfill State Registration Requirements
Most states require you to register your AED with local emergency services or a specific state agency. This is a critical step that connects your device to the 911 system. When someone calls 911 to report a cardiac arrest near your location, the dispatcher can see your registered AED and direct the caller or first responders to it. This simple act can save precious minutes and turn your device into a community asset. Because AED laws vary by state, you’ll need to identify and follow your specific local requirements to ensure you’re fully compliant from day one.
Secure Medical Director Oversight
Medical oversight means having a licensed physician oversee your AED program. This doctor provides a prescription for the device (if required), approves your emergency response protocols, and reviews event data if the AED is ever used. This oversight ensures your program aligns with current medical best practices and adds a powerful layer of credibility and liability protection. Many states mandate medical oversight as part of their Good Samaritan laws. It demonstrates that you’re not just installing equipment, but implementing a medically sound emergency response plan under professional guidance.
Keep Your Documentation Audit-Ready
If an inspector or attorney asked you to prove your AED was working last Tuesday, could you? Keeping your documentation audit-ready means maintaining meticulous records of everything related to your device. This includes routine inspection logs, battery and electrode pad expiration dates, and staff training certificates. These records are your proof of due diligence, showing that you consistently maintain your device according to the manufacturer’s specifications. A well-organized logbook—whether physical or digital—is essential for demonstrating compliance and protecting your organization. Using a system that automates readiness monitoring and compliance ensures your records are always current and accessible.
How Installation Varies by Facility Type
Where you install your AEDs depends entirely on your environment. A sprawling corporate campus has different needs than a local elementary school, and state or industry regulations often dictate specific requirements for certain types of facilities. Thinking through the unique risks and traffic patterns of your location is the first step toward creating a placement strategy that makes sense.
Your goal is to place AEDs where a sudden cardiac arrest is most likely to occur and where responders can get to the device quickly. This means considering high-traffic hallways, areas where people exert themselves physically, and locations with a higher concentration of at-risk individuals. A well-managed AED program accounts for these variables to ensure your devices are always where they need to be when an emergency strikes. Let’s look at a few common facility types and their specific installation needs.
Schools and Campuses
Schools are bustling with activity, from crowded hallways and cafeterias to athletic fields and gymnasiums. To protect students, staff, and visitors, AEDs should be placed in central, high-traffic locations that are accessible during and after school hours. Many states have specific laws mandating AEDs in schools, and the trend toward required placement is growing globally. For instance, some countries now require that all schools have at least one defibrillator. Placing devices near gyms, auditoriums, main entrances, and the nurse’s office ensures they are ready for any emergency, whether it happens during a basketball game or a parent-teacher conference.
Offices and Corporate Buildings
In a corporate setting, protecting your employees and visitors is a top priority. While specific laws vary, OSHA encourages workplaces to have AEDs available as part of a comprehensive first-aid program. For large, multi-story buildings, a good rule of thumb is to have at least one AED on each floor, especially near elevators, break rooms, or other central gathering spots. This strategy minimizes the time it takes for someone to retrieve a device, which is critical during a cardiac emergency. A visible and accessible AED shows your team you’re invested in their well-being and prepared to act when seconds matter most.
Gyms and Healthcare Facilities
Some locations carry a higher risk of sudden cardiac arrest, and gyms are at the top of that list. The physical exertion that happens in fitness centers makes them a prime location for cardiac events, which is why many states have laws requiring them to have AEDs on-site. According to one AED placement guide, “places in a building are more likely to have a cardiac arrest, like gyms or very crowded rooms. These areas should have AEDs nearby.” Similarly, healthcare facilities must be equipped to handle medical emergencies. Many states, like Louisiana with its Jump Start Your Heart Act, have specific legislation requiring AEDs in these environments.
How to Handle AED Maintenance and Inspections
Installing an AED is a fantastic first step, but the work doesn’t stop there. An AED is only effective if it’s ready to work at a moment’s notice, and that readiness depends entirely on ongoing maintenance. Neglecting inspections is one of the most common and dangerous mistakes organizations make. Without them, you risk having a device with a dead battery or expired pads that fails during a cardiac arrest emergency, which undermines the entire reason for having it in the first place. This not only creates a false sense of security but can also expose your organization to significant liability.
Proper maintenance isn’t complicated, but it does require consistency and attention to detail. It boils down to three core practices: performing routine visual checks, tracking the expiration dates of critical components, and using modern tools to automate readiness monitoring. Think of it like maintaining a fire extinguisher; you need to know it will work before you ever need it. By building these habits into your safety plan, you can feel confident that your AED is prepared to save a life when every second counts. Our approach to AED program management is built around these key pillars.
Follow a Routine Inspection Schedule
Regular inspections are the foundation of a reliable AED program. Most manufacturers recommend checking your device at least once a month. During this check, you’ll want to confirm the green status indicator is lit or flashing, which signals the AED has passed its last self-test. You should also check that the device is clean, unobstructed, and that rescue supplies like razors and gloves are present. Documenting every inspection is crucial for compliance and creates a clear record of readiness. A simple logbook kept near the AED can work, but a centralized digital system is even better for tracking multiple devices.
Track Battery and Pad Replacements
Your AED’s battery and electrode pads are the two components that absolutely must be replaced on a schedule. These items have a limited shelf life, typically lasting between two and five years, and they will expire whether the AED is used or not. It is crucial to monitor these expiration dates and order replacements well in advance. Forgetting to do so is a primary cause of AED failure during an emergency. If you manage multiple AEDs across different locations, manually tracking these dates can become a serious administrative challenge. This is where having a partner to manage your AED lifecycle can prevent critical supplies from falling through the cracks.
Use Remote Monitoring and Alerts
The most effective way to guarantee your AED is always ready is to use technology that does the checking for you. Modern AEDs can connect to remote monitoring systems that provide real-time status updates. These systems automatically perform daily, weekly, and monthly self-tests and will send you an immediate alert via email or text if an issue is detected. You’ll be notified if the battery is low, if pads are nearing their expiration date, or if the device fails a self-test for any reason. This technology removes the risk of human error and the burden of manual inspections, giving you complete confidence that your AED is functional and compliant 24/7.
What Costs Should You Expect?
When you’re planning for an AED program, the price of the device itself is only the beginning. To create a reliable and compliant program, you also need to account for ongoing costs like battery and pad replacements, training, and program management. Understanding the total financial commitment from the start helps you make the best decision for your organization’s budget and goals. The primary choice you’ll face is whether to purchase your AEDs outright or enroll in a rental program. Each path has different implications for your budget, so let’s break down what you can expect.
Buying vs. Renting an AED
Purchasing an AED is a capital expense, and it can be the more cost-effective option if you plan to keep the device for more than five years. When you buy, you own the asset completely. However, ownership also means you’re responsible for every associated cost down the line, including replacing supplies and eventually the device itself. On the other hand, an AED rental program turns that large upfront investment into a predictable, manageable operating expense. Renting often bundles the hardware, routine maintenance, and supply replacements into one recurring fee. This approach keeps your program financially flexible and eliminates the surprise costs that can come with long-term ownership, making it easier to budget accurately year after year.
Budgeting for Maintenance and Compliance
Whether you buy or rent, ongoing maintenance is not optional—it’s essential for keeping your device ready and your organization protected. If you purchase your AED, you’ll need to budget separately for replacing electrode pads and batteries, which expire every two to five years. You are also responsible for tracking these dates and performing routine inspections to stay compliant. This is where a rental or a managed service plan simplifies everything. Most rental agreements include automatic supply replenishment and service reminders, so you never have to worry about an expired battery. With comprehensive program management, all compliance tasks—from monthly checks to medical oversight—are handled for you. This removes the administrative burden and ensures your program is always audit-ready.
Avoid These Common AED Installation Mistakes
Placing an AED in your facility is a critical step toward protecting your team and visitors, but the work doesn’t stop there. A few common missteps can make your device ineffective when you need it most. From poor placement to forgotten maintenance, these oversights can undermine your entire emergency preparedness plan. By understanding these potential pitfalls, you can ensure your AED program is not just compliant, but truly life-saving. Let’s walk through the most frequent mistakes and how you can easily avoid them.
Inaccessible or Hidden AEDs
An AED can’t save a life if no one can find or reach it in time. One of the biggest mistakes is placing a device in a locked office, a cluttered storage closet, or an out-of-the-way corner. Your AED should be installed in a visible, central, and high-traffic location where people gather, like a lobby, cafeteria, or main hallway. It’s also essential to follow ADA accessibility guidelines to ensure the cabinet is at a height that everyone, including individuals in wheelchairs, can reach. Clear, bold signage pointing the way to the AED is just as important as the device itself, guiding responders quickly and confidently during a high-stress emergency.
Neglecting Training and Documentation
Simply having an AED on the wall isn’t enough—your team needs the confidence to act. While modern AEDs are designed for ease of use, hands-on training removes hesitation when seconds are critical. Effective training programs should cover more than just the device; they must include CPR certification and a clear emergency response plan so everyone knows their role. Forgetting to document who was trained and when can also create compliance gaps. Keeping detailed records not only prepares your team but also ensures your program is organized and ready for any audit, protecting both your people and your organization.
Skipping Routine Maintenance Checks
An AED is a medical device that requires regular attention to stay ready for use. It’s easy to assume it’s fine until it’s needed, but batteries and electrode pads expire, and device errors can occur. A responsible person should perform routine visual inspections to check the status indicator light and confirm that supplies are within their expiration dates. Without consistent oversight, you risk having a non-functional device during an emergency. A comprehensive AED program management system automates these checks and reminders, giving you peace of mind that your device is always prepared to function as expected.
Related Articles
- AED Laws & Requirements Across State — AED Total Solution
- AED Cost Explained – Your Questions Answered
- Why is Defibrillation Important – Legal Guidelines
- True AED Cost Explained: Real Prices, Fees & Buying Guide — AED Total Solution
- AED Program Management | Compliance and Maintenance
Frequently Asked Questions
My AED gives voice instructions. Why is formal training still necessary? While modern AEDs are incredibly user-friendly, the real value of training is building the confidence to act without hesitation. An emergency is a high-stress situation, and formal training provides the hands-on practice needed to overcome the initial shock and panic. It teaches your team how to recognize the signs of cardiac arrest, perform effective CPR, and work together seamlessly, ensuring the entire response is fast and correct long before the AED’s voice even begins guiding them.
What are the biggest legal risks if I don’t manage my AED program correctly? The biggest risk is losing the liability protection offered by Good Samaritan laws. These laws are designed to protect organizations that act in good faith, but that protection often depends on responsible program management. If you neglect to register your device with local EMS, fail to perform and document routine maintenance, or don’t have proper medical oversight, you could be seen as negligent. This leaves your organization vulnerable if something goes wrong.
Is one AED enough for my building? It depends on whether a rescuer can grab it and return to the victim in under three minutes. The best way to know for sure is to physically walk the path from the farthest point in your facility to the proposed AED location and back again. If that round trip takes longer than three minutes at a brisk pace, you need another device to cover that area. Remember to account for real-world barriers like stairs, locked doors, or crowded hallways that can slow someone down.
What are the “hidden costs” of owning an AED? The initial purchase price is just the first expense. The ongoing costs include replacing the battery and electrode pads, which expire every two to five years, regardless of use. You also need to budget for recurring CPR and AED training for your staff to keep their certifications current. Finally, there’s the administrative cost of the time your team spends performing monthly inspections, tracking expiration dates, and maintaining compliance records.
I’ve installed our AED. What are the most important things I need to do now? Your immediate next steps are to handle the administrative side of your program. First, make sure you complete any required state or local registration for your device so 911 dispatchers know it exists. Next, establish a consistent maintenance schedule for monthly inspections and create a system to track battery and pad expiration dates. Finally, schedule CPR and AED certification for your key staff members and develop a clear emergency response plan so everyone knows their role.
Disclaimer for information purposes only:
The information provided on this website is intended for general educational and informational purposes only. It is not medical advice and should not be used as a substitute for professional diagnosis, treatment, or care. Always consult a qualified healthcare or medical professional regarding any health-related questions or concerns.
While we strive to ensure the information shared is accurate and up to date, no guarantees are made regarding completeness, accuracy, or applicability to any individual situation. Use of this content is at the reader’s sole discretion and risk.
This website is part of the Response Ready family of emergency preparedness and training resources, including CPR & first aid training and compliance services, AED sales and program support, AED program management software, and medical oversight solutions provided through our affiliated platforms:
• CPR1.com
• AEDLeader.com
• ResponseReady.com
• MDSIMedical.com
By accessing or using this website, you agree to release, indemnify, and hold harmless the website owners, authors, contributors, and affiliated entities from any claims, losses, damages, or liabilities arising from the use or reliance on the information presented.